Case Studies
Providing the highest standard of professional care in a friendly, comfortable environment.
Case Studies
Providing the highest standard of professional care in a friendly, comfortable environment.
Complex Anatomy
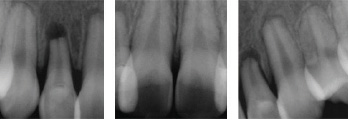
Dilacerated Roots
The patient also admitted they have a “hard time getting
numb.” Before starting treatment, the anesthesia was
supplemented with an x-tip intraosseous injection in
the 3rd molar region to ensure a pain free experience.
The dilacerated canals were carefully negotiated and
debrided to length using Pathfiles (Tulsa) and Twisted
(Sybron Endo) rotary files. Note the 90 degree sharp
dilaceration of the distal root.


Complex Anatomy
180 Degree MB Root Curvature
This patient required root canal treatment of tooth #26.
We saw him 5 years earlier for treatment of
tooth #27 and knew the curvatures were going to
be challenging. With the help of the microscope and
extremely flexible nickel-titanium instrumentation, all
4 canals were treated to length. Note the separate
portal of exits for the MB and MB2 canals. More
importantly, note the 180 degree curvature of the
MB2 canal.


Complex Anatomy
3 Canal Premolar
The patient’s chief complaint was cold sensitivity in the lower left.
After a thorough clinical and radiographic exam the
pain localized to tooth #35. The Pre-Op x-ray revealed
a 3 rooted anatomical variant. The tooth was accessed
and with the help of the microscope’s 16x magnification
the MB, DB and P canals were debrided, disinfected,
and obturated. Studies have shown that less than
1% of lower premolars have 3 or more canals.


Complex Anatomy
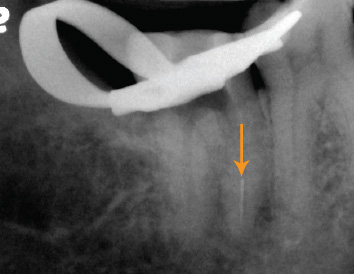
Severe Dilaceration
This patient was accommodated for same day
emergency root canal treatment of tooth #37 at the
request of the referring office. The inflamed pulp was
successfully debrided, disinfected, and obturated.
Note the severely dilacerated distal canal!


Retreatment
Separated Instrument Removal
A referral was made to our office to try and save tooth #37.
There was a separated instrument in the ML canal around a sharp root curvature. The apex of the tooth also had a large rarefying osteitis. The broken instrument was first isolated by enlarging the canal above it. We were then able to visualize the instrument using 16x magnification and successfully removed it using specialized ultrasonic instrumentation. All 3 canals were then debrided, disinfected and obturated. Note the bone regeneration at the 1 year follow up. The patient and referring dentist were extremely happy with the final result.






Retreatment
Separated Instrument Removal
Patient was referred due to persistent bite pain on tooth #47.
There was a separated instrument in the MB canal that was successfully isolated and removed with the help of micro-ultrasonic instrumentation. The
MB and ML canals ultimately joined and the canals were obturated with gutta percha and BC Sealer. At the 6 month follow up the patient was asymptomatic
and a crown was advised.




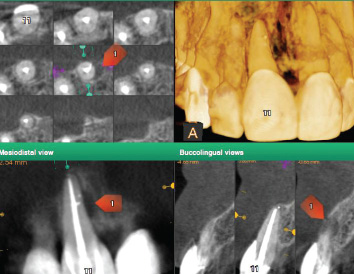
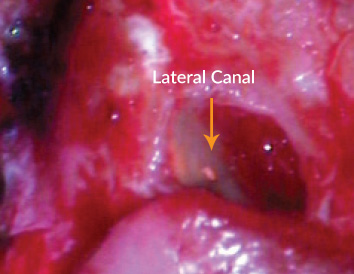
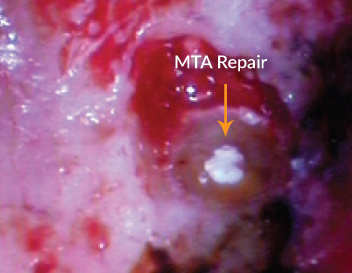
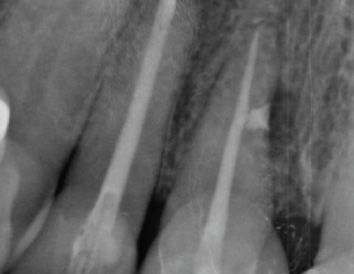
CBCT
Surgical Repair Of A Lateral Canal
This patient was experiencing pain to palpation on the buccal of tooth #11 but the Pre-Op x-ray was inconclusive.
The CBCT scan was able to isolate the lesion to a lateral canal on the mesial root surface. A full thickness submarginal flap was raised and after curetting
the lesion the lateral canal was visualized with 16x magnification. The lateral canal was then prepared and filled with Mineral Trioxide Aggregate. The flap was sutured and a Post-Op image taken. Note the radiographic healing (bone regeneration) at the 1 year follow up. Thanks to CBCT technology we were able to
properly diagnose and treat tooth #11.


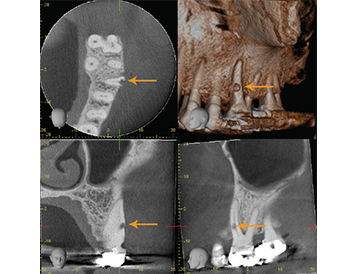
CBCT
External Resorption
The patient developed a draining sinus tract on the buccal of tooth #26.
The confusing part was that the pulp was still testing vital (normal). We took a CBCT scan and discovered external cervical root resorption on the buccal surface of the MB root. Extraction was advised, given the location of the defect and the associated periodontal pocket. The use of CBCT technology saved this patient from unnecessary exploratory treatment.


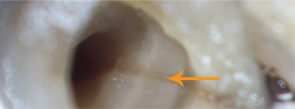
Crack Diagnosis
Vertical Fracture
This patient’s chief complaint was occasional sharp pain to biting.
The crack tooth syndrome localized to tooth #47. An x-tip intraosseous injection was used in the 3rd molar region to supplement the anaesthesia. The restoration was removed and a crack was noted extending from the distal marginal ridge. After a full pulpectomy, the crack was visualized with 12x magnification extending deep into the distal canal. The long-term prognosis was hopeless and the patient was referred back to her dentist for extraction of tooth #47.


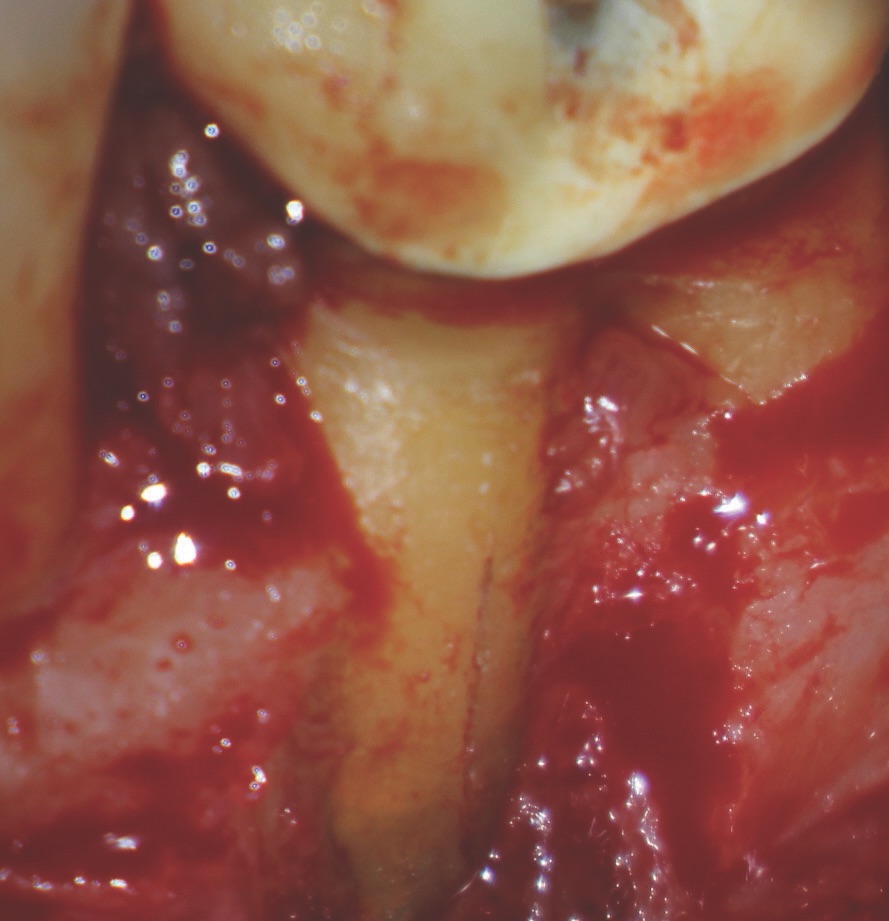
Crack Diagnosis
Vertical Root Fracture
An apicoectomy was advised for tooth #36 due to
persistent pathology at the mesial root apex. A full
thickness sulcular flap was raised and with the help of
the microscope the root fracture was detected. Vertical
root fractures have a hopeless prognosis. The flap was
repositioned with sutures and the patient was referred
back to his dentist for extraction. Without the help of the
microscope this root fracture would have never been seen.

Trauma
Extrusive Luxation
The patient was seen at our office for emergency treatment after being in a physical altercation after school. Teeth #12,11,21, and 22 were luxated and extruded in the palatal direction. No evidence of an alveolar fracture was present. The teeth were repositioned using anterior extraction forceps and digital pressure. Semi rigid splinting with a 20guage ortho wire and flowable composite was completed. The splint was removed after 3 weeks and long term follow up was advised. After 6 months, the pulps tested non-vital and root canal therapy was completed. At the 1 year follow up there was complete radiographic healing and the patient was asymptomatic and extremely grateful she could save her front teeth.